by Merridee Lefner, Graduate Student, UTSA Neuroscience Institute
On Monday the 10th of April, The University of Texas at San Antonio’s Neurosciences Institute welcomed a lecture by Dr. D. James Surmeier on a strategy for slowing the progression of Parkinson’s Disease (PD). PD affects more than 1.5 million people in the United States, and is the second most common neurodegenerative disease in the developed world. As life expectancy continually increases, the amount of people expected to suffer from this age-related disease is predicted to skyrocket. Slowness of movement, rigidity, and resting tremor are some of the major motor symptoms of PD, and while some symptomatic treatments are available, we have yet to find a way to slow or stop the disease. Dr. Surmeier is attempting to bridge the gap between basic science and clinical practice in hopes to modify the progression of PD.
A Hypothesis for the Cause of PD
The motor symptoms associated with PD has been causally associated to the loss of dopaminergic (DA) neurons located in the substantia nigra pars compacta (SNc). These DA neurons innervate the basal ganglia, which controls movement and action selection. The basal ganglia circuitry is around 500 million years old, and may be the reason we have survived as long as we have: it organizes our behavioral response to challenging threats, so that we may successfully escape dangerous situations. Because of this, the DA neurons in the SNc are constantly active. The neurons are tonic pacemakers due to calcium entry into the cell via the opening of plasma membrane Cav1 calcium channels. This promotes calcium entry into the mitochondria, stimulating oxidative phosphorylation and the production of ATP. This ensures that bioenergetic needs are met, although it may come at a cost: the high demand for ATP can lead to mitochondrial oxidant stress. Sustained mitochondrial oxidant stress could result in increased turnover by mitophagy, causing cell aging and death. Surmeier points out that other PD-affected brain regions also exhibit pacemaking activity, Cav1 calcium channel expression, and mitochondrial oxidant stress.
A Possible Treatment
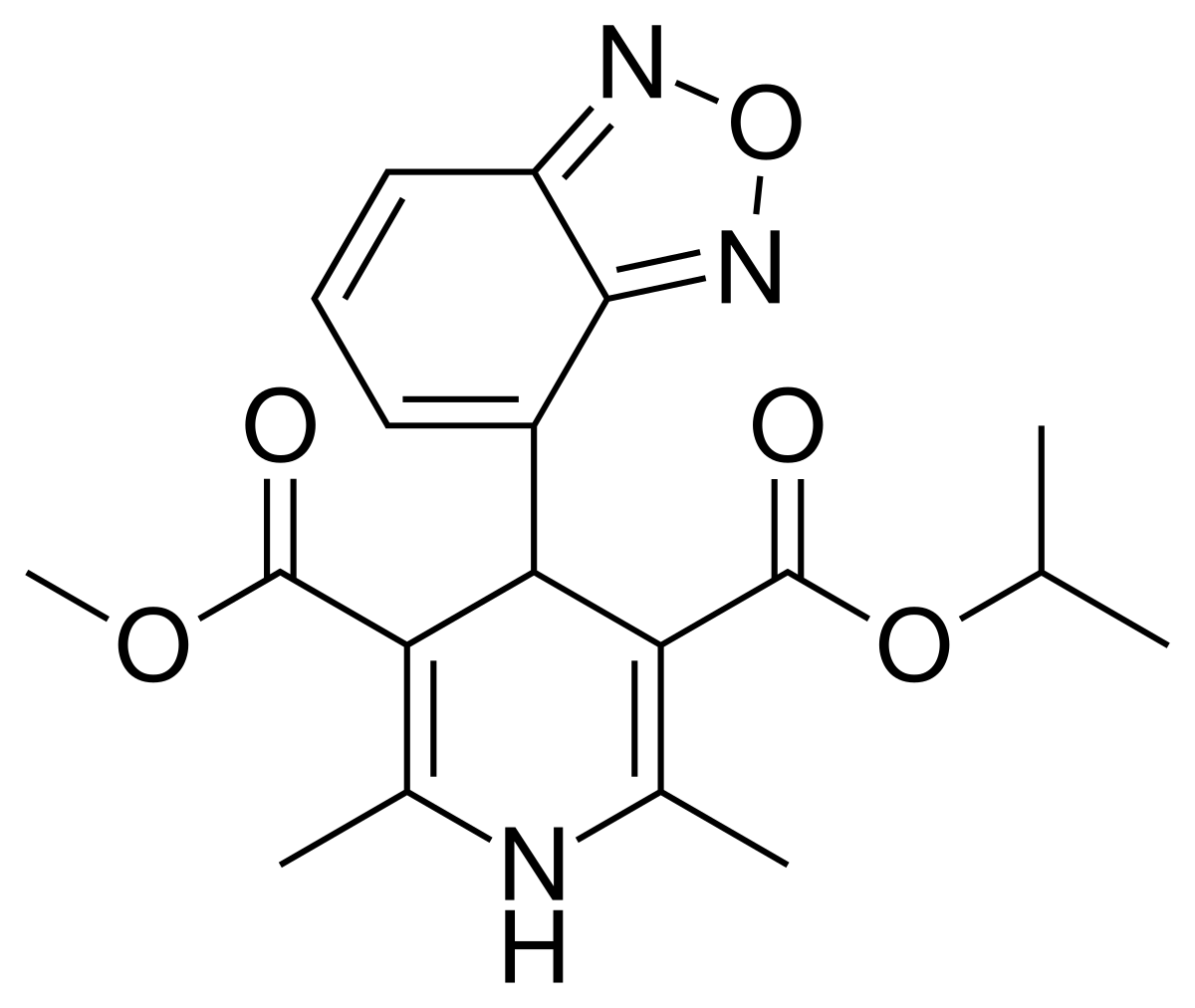
Parkinson’s Disease is a modern problem, because human life expectancy has only recently increased by about 60 years, allowing us to live long enough to reach the age of PD onset. We no longer live in the same dangerous environment that humans were once required to survive in, so maybe we don’t need the SNc neurons to work as hard as they were originally meant to be. So, can we remodel these neurons in a way that allows them to take a break, without compromising their ability to do their job in the less threatening and more predictable world we live in today? Surmeier noticed that isradipine, a drug initially used to treat cardiac hypertension, decreased the risk PD diagnosis by about 30% and resulted in slower disease progression if diagnosed. He found that isradipine acted as a negative allosteric modulator for Cav1 calcium channels. When mice were systemically treated with isradipine, Surmeier observed lowered intracellular calcium levels, lowered mitochondrial oxidant stress, lowered mitochondrial damage and mitophagy, and increased mitochondrial mass. This indicates that isradipine treatment could provide relief towards mitochondrial oxidant stress, which may help slow PD progression.
Phase III Trials with Isradipine
One issue with Surmeier’s findings is that his experiments were performed in mice, and there is no existing mouse model of PD. However, human brains show telltale signs of sustained mitochondrial oxidant damage, suggesting that the effect of the stress is similar in humans. Surmeier conducted a Phase II study on early stage PD patients to determine the tolerability of isradipine and found it to be well-tolerated at doses below 10 mg/day. Now, Phase III clinical neuroprotection trials sponsored by the National Institutes of Health will determine whether three years of isradipine treatment could slow the progression of PD in recently diagnosed patients. The study will be complete in 2019. Since it is not possible to start treatment before the symptoms of PD appear, patients will already have lost a significant fraction of their SNc dopaminergic neurons. The hope is that isradipine treatment will extend the survival of the remaining neurons by relieving mitochondrial stresses. Ultimately, this could have a profoundly positive impact on the quality and duration of life of these patients, in addition to the obvious benefits in terms of limiting health care costs.
Dr. D. James Surmeier
Dr. D. James Surmeier is a Nathan Smith Davis Professor and Chair of Physiology at the Feinberg School of Medicine at Northwestern University. He is a leading authority on the fundamental mechanisms of Parkinson’s Disease, a member of various prestigious scientific societies, and recipient of numerous scientific awards. He directs the Morris K. Udall Center of Excellence for Parkinson’s Disease at Northwestern University, one of 9 elite, multi-disciplinary centers funded by the National Institutes of Health to concentrate on causes and cures for Parkinson’s Disease. The research in his lab focuses on how neuromodulators shape the excitability of basal ganglia and frontal cortex neurons. These two areas share a rich monoaminergic innervation arising from the mesencephalon and medulla, and disorders in signaling in these forebrain structures have been implicated in a wide variety of psychomotor disorders such as Parkinson’s disease.
Surmeier, DJ, Schumacker, PT, Guzman, JD, Ilijic, E, Yang, B, Zampese, E (2016). Calcium and Parkinson’s disease. Biochemical and Biophysical Research Communications 483, 1013-1019. The Journal of Neuroscience (2016).
Author Bio: Merridee Lefner is a first year graduate student studying the role of dopamine in motivated behavior in the Neurobiology program at the University of Texas at San Antonio. She built a relationship with the Mind Science Foundation through their support of UTSA’s Neurobiologists Evolving Undergraduate Research Opportunities (N.E.U.R.O.) Club where she served as president. Merridee loves the brain and hopes to one day have her own lab!